Preventing Contact Lens Dropout and Complications
Practical approaches to prevent common issues related to lens wear.
 Jessica O. Yu, OD, FAAO, FSLS
Jessica O. Yu, OD, FAAO, FSLS
As many as one in four patients drops out of contact lens wear in the first year.1 According to research commissioned by the Contact Lens Institute last August, which included 401 US adults split equally between new (< 2 years) and long-term (≥ 2 years) soft contact lens wearers, the top five reasons for dissatisfaction with contact lens wear that led to discontinuation of wear were cost, handling, comfort, vision, and convenience (Figure).2 However, with today’s ever-evolving contact lens technology and some proactive measures taken on our part, we should easily be able to address these reasons. Contact lens-related complications, on the other hand, are another matter. Most can be prevented, but others will rear their ugly heads when we least expect it, no matter how careful we try to be. In these situations, we strive to find the best solutions and continually learn from our experiences. This article focuses on these common contributing variables affecting the satisfaction and success of our contact lens patients.
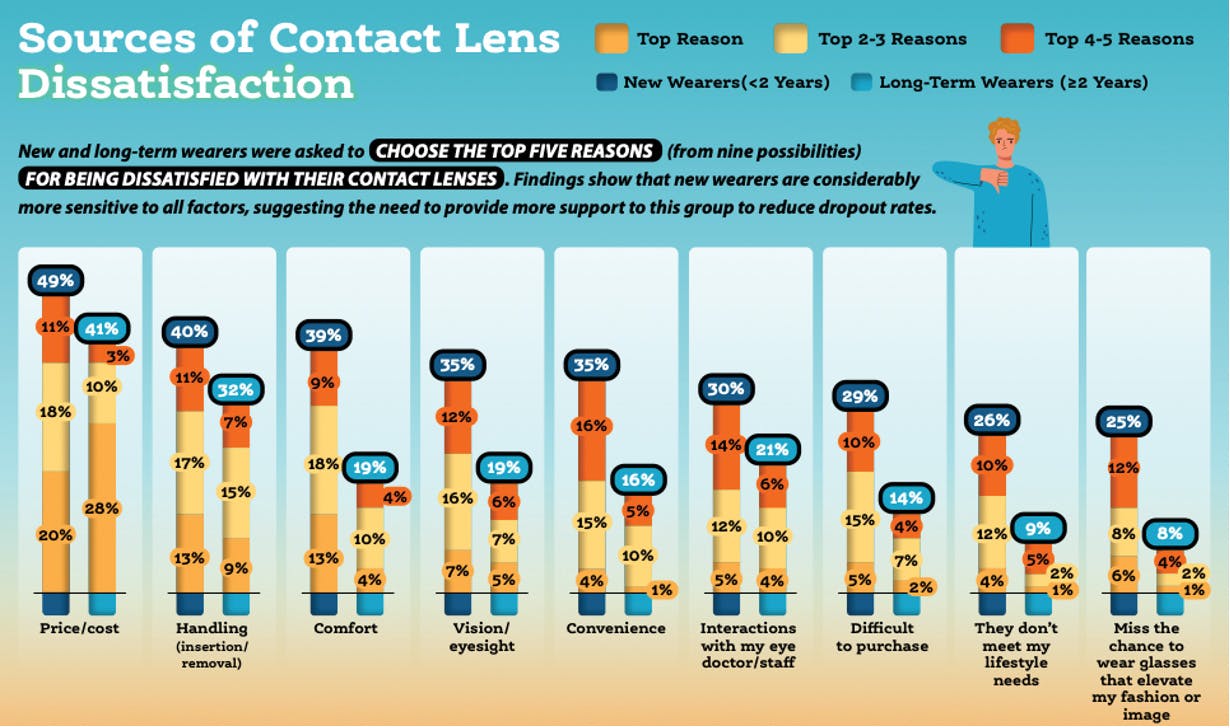
Figure. Sources of dissatisfaction in US adults 18 to 64 years of age who reported wearing soft contact lenses at least once per week. New wearers n = 200; long-time wearers n = 201. Figure courtesy of the Contact Lens Institute.
DEALING WITH DROPOUT
Providing thorough explanations and setting proper patient expectations go a long way when it comes to managing costs, comfort, vision, and convenience as they relate to contact lens wear. Below, I’ll review the key areas that contribute to contact lens dropout.
Costs
For some patients, the expense of contact lenses themselves, along with solutions, eye exams, and the separate fitting fee, can seem costly and may be enough to deter them from contact lens wear altogether. Others may drop out of contact lens wear because they find these costs to be burdensome over time. While the cost of eye care varies by region, you can try to temper cost-related dissatisfaction in your patients by setting expectations the first time you have a conversation about contact lens wear. Be sure to discuss the pros and cons of wear, why it’s important they order their lenses from a licensed eye care provider, and what options and rebates are available that may affect price. Most importantly, it is an opportunity for us as eye care professionals to build value in the fitting process and what we do.
Handling
Contact lens handling issues such as poor hygiene, improper techniques, and ineffective lens cleaning can cause corneal abrasions or infections and even lead to patients dropping out of lens wear. Depending on what I see in the patient history and what I hear from the patient as I ask more specific questions about their habits, I may choose to have a more in-depth discussion with them on certain points. For example, if I notice deposits on a patient’s monthly replacement lenses and they tell me they use a generic multipurpose solution, I’ll say, “So, you told me you’re using solution X, but for your lens, a more compatible and advanced solution to clean with would be solution Y.” And then I’ll review the steps, explaining that when they remove their lenses, they should give them a 5-second rub. (I’m a big fan of rubbing reusable lenses because the digital manipulation removes a lot of deposits that tend to build up, whether from environmental factors or from the patient’s own tear chemistry.) I’ll also remind them to replace their lens case once a month or every time they buy a new bottle of solution because some people don’t realize the case has its own lifespan.
Comfort
The most basic comfort questions to ask a patient are what contact lens they last wore and what their experiences were with it. It’s important to drill down and get specific. Did they explore different types of lenses, different brands, or different materials? Did the lens become uncomfortable shortly after insertion or towards the end of the day? With modern contact lens technology, it’s rare for a lens to get so tight that it becomes uncomfortable for a patient, but it can happen. Loosening the fit, adjusting the base curve or diameter, and/or changing the material can affect how the lens feels when a patient gets to hours 6 to 8 and beyond.
It’s rare for patients wearing daily lenses to complain of comfort issues, but there are the occasional issues of dryness, discomfort, and material sensitivity. In such cases, I always ask patients what they’re rinsing with and personally recommend they use PuriLens Plus Saline (The LifeStyle Company). There are other preservative-free solutions available, such as Sensitive Eyes Saline Solution (Bausch + Lomb), but I like the PuriLens Plus.
Contact lens cleaning and care play a big factor in comfort, although this obviously pertains to reusable lenses. When you have a patient in reusable lenses who has tried everything with no improvement, a hydrogen peroxide system like Clear Care (Alcon) can eliminate a lot of sensitivities and comfort issues.
Ocular Surface Issues
Patients who complain of dry eye present a great opportunity to refit them into a daily disposable if they are not already wearing this modality. Another option is to move them from a hydrogel daily disposable to a silicone hydrogel or a better technology daily disposable lens.
Regarding the replacement schedule, it should be noted that for patients who are on, especially, monthly lenses, that 1-month timeframe is the maximum use of the lens, not the minimum. Many people will think, “it’s a monthly, so I have to hit that monthly point.” But for some people, the lens simply isn’t as comfortable in the latter half of the cycle, and they shouldn’t feel compelled to just push through. Based on their eyes and tear film chemistry, the lens, the season, or their coexisting issues, patients sometimes have to be told it’s okay to wear a monthly lens for only 3 weeks, throw it away, and start fresh.
When it comes to seasonal allergies, you have to treat them concurrently, and I always remind patients that allergy drops can’t be used while wearing contact lenses. (A surprisingly high percentage of people don’t realize you shouldn’t be instilling these medications with lenses in, because you don’t want the lens acting like a sponge and absorbing the different chemicals, which could potentially create corneal toxicity problems and contribute to contact lens discomfort.) Many people overuse allergy drops and don’t realize that it can increase dryness symptoms. Likewise, oral antihistamines can have a similar effect in increasing dryness, so treatments for both types of symptoms have to be balanced. This is a good time to inform or remind patients that only a few lubrication drops are contact lens compatible (Table) and that most should not be instilled while wearing lenses. Consider this an opportunity to refit a patient with allergies—and even those with concomitant dry eye—into daily disposable contact lenses.
Vision
Patients with astigmatism or presbyopia may achieve less-than-ideal vision with contact lens wear, which can lead to dissatisfaction and, ultimately, dropout. Additionally, patients with complex prescriptions—that is, those who need or want to wear lenses, but their prescription limits them in some way—can also be easily discouraged with lens wear. It’s a bit of a theme here, but a great way to try to head off any disappointment is to set realistic expectations. Let patients know that only so many companies make lenses that will fit their prescription and perform the way they want and/or need them to perform. If a patient understands this, hopefully they will be willing to take the extra steps to ensure they get the best wearing experience.
Convenience
Contact lenses as a vision-correction option in general are more convenient than glasses because they don’t fog up or slide down, and you can wear nonprescription sunglasses with them. They’re also more convenient for active individuals. Within the contact lens category, daily replacement lenses are not only the most convenient, but they are also best for cleanliness, eye health, and minimizing potential issues. As a practitioner, they are my go-to contact lens modality for my patients. I wouldn’t recommend anything else.

PREVENTING DROPOUT AND COMPLICATIONS
With my mind on preventing contact lens dropout and complications, I start my contact lens exams with a thorough history to learn about the patient’s habits, what’s working, and what’s not working. From there, I’ll build through my examination, which entails getting a sense of their vision, their prescription, and any binocular issues. I then perform a thorough slit-lamp exam to evaluate all of the external ocular components (ie, lids, lashes, tear film). I don’t just observe the quality of the tear film, but also the quantity—how thick or thin is it? Is it a little spotty? Oily? Looking at those components tells me how their tear film could affect them as a contact lens wearer. From here, I base their prescription on what they’re looking to achieve with their contact lenses and how they would ideally like to use them. So, if they’re presbyopic and want to wear contact lenses to do everything in their life, then a multifocal is a great option. If a patient needs a toric lens because they’re astigmatic, that drives the type of lens I choose to fit them with. Then I try my best to ensure they understand why I am selecting that lens for them and why I think it’s the best choice. It’s about educating them on the different points relating to contact lens wear (eg, hygiene, risk of infection, lens feature, or material benefits).
Then, on slit-lamp or physical examination, if I see anything, such as redness, edema, neovascularization, or other signs that show the eye is more agitated, I will ask if they sometimes sleep in their lenses. This will prompt me to dig deeper and look back to the history.
A lot of busy adults underestimate the value of taking their lenses out right away when they feel something is off, and that’s a big reason why we see the infection or abrasion rates that we do. When we’re teaching new wearers how to use contact lenses, we always tell them, “When in doubt, take them out.” Since I’ve been practicing, the incidence of infections—bacterial keratitis, Acanthamoeba, fungal infections, etc—and hypoxic situations has decreased significantly thanks to the increased popularity of daily disposable lenses, as well as improvements in contact lens materials, breathability, and oxygen permeability over the past decade and a half. Most contact lens-related infections these days are tied to patients who overwear their extended wear or misuse daily wear lenses.
RETENTION IS IN THE DETAILS
Contact lens dropout can affect a practice’s profitability due to lost revenue, which is why it’s important to understand and address the different factors that lead to patient dissatisfaction with their lenses. Never underestimate the importance of careful patient selection, setting realistic expectations, ensuring proper lens care and hygiene, and proactively addressing potential complications.
References:
- Sulley A, Young G, Hunt C. Factors in the success of new contact lens wearers. Cont Lens Ant Eye. 2017;40(1):P15-P24.
- Disrupting the dropout dilemma: practical steps to keep patients in contact lenses. Contact Lens Institute. See Tomorrow Contact Lens Institute. Fall 2024. Accessed April 7, 2025. www.contactlensinstitute.org/wp-content/uploads/2024/10/CLI-Disrupting-Dropout-Report_Fall-2024_FINAL.pdf
Jessica O. Yu, OD, FAAO, FSLS
Optometrist, Connecticut Contact Lens Institute, Fairfield County, Connecticut
jessicayuod@gmail.com
Financial disclosure: Consultant and Speaker (Bausch + Lomb)
Ready to Claim Your Credits?
You have attempts to pass this post-test. Take your time and review carefully before submitting.
Good luck!






